Program Overview
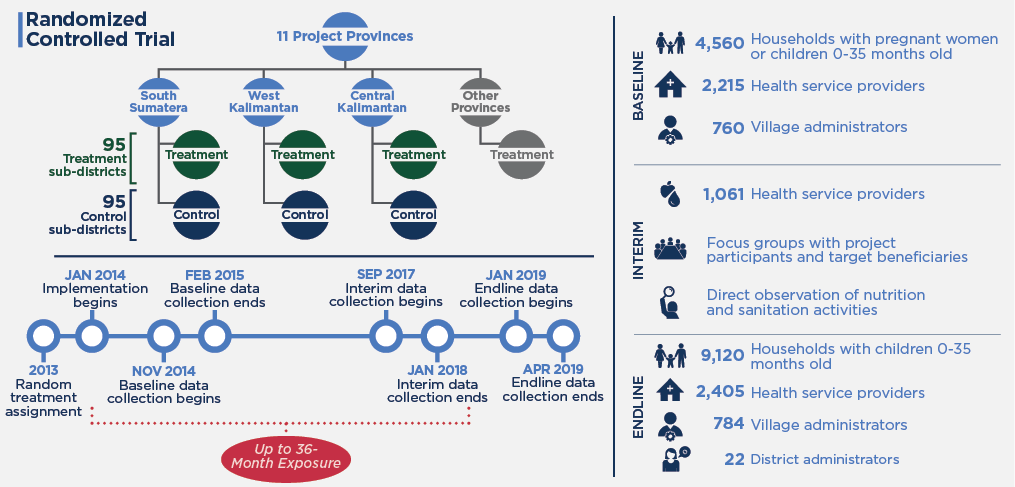
MCC’s $474 million Indonesia Compact (2013-2018) funded the $120 million Community-Based Health and Nutrition to Reduce Stunting Project. The Nutrition Project aimed to avert undernutrition of children in 11 provinces. It trained health workers on infant and young child feeding, growth monitoring, and sanitation; conducted community sanitation events; provided iron-folic acid to pregnant women; conducted a communications campaign on stunting; and provided grants to incentivize the use of health services through Generasi, a community-driven development program.
Evaluator Description
MCC commissioned an independent final impact evaluation of the project by Mathematica. Full report results and learning: https://data.mcc.gov/evaluations/index.php/catalog/109.
Key Findings
Nutrition Project Objective
- The Nutrition Project did not achieve its long-term objective of impacting child undernutrition, as measured by child stunting, wasting, underweight, or low birthweight.
Sanitation-Related Intermediate Outcomes
- The Nutrition Project had a positive impact on the percentage of villages that were “triggered” (through interactive community gatherings) to eliminate open defecation, but had no impact on villages becoming open-defecation free.
- There was also no impact on household sanitation facilities, sanitation behaviors, or the incidence of diarrhea—outcomes that were expected to contribute to reduced undernutrition.
Nutrition-Related Intermediate Outcomes
- The Nutrition Project had little effect on receipt of one-on- one counselling from health providers by pregnant women and caregivers of young children, and only a modest impact on attendance at nutritional group counselling sessions.
- Improvement in health behaviors that could contribute to reducing undernutrition was modest; the project had positive impacts on iron and folic acid (IFA) consumption during pregnancy, exclusive breastfeeding, and child meal frequency.
- The analysis did not identify any patterns that suggested that impacts were systematically different for particular subgroups.
Evaluation Questions
This final impact evaluation was designed to answer the following questions:
- 1
What is the impact of the Nutrition Project’s package of supply- and demand-side activi- ties on key outcomes, including: behavioral practices (sanitation, breastfeeding, complementary feeding, food diversity, and IFA consumption); receipt of health services (nutritional counseling, growth monitoring, prenatal and postnatal care, vaccination, and vitamin supplementation); and child health outcomes (stunting, wasting, underweight, birthweight, diarrhea, and worms)? - 2
Which demand-side and supply-side ele- ments were the key drivers of impacts? - 3
What is the impact of the Nutrition Project on key subgroups, such as those defined by socioeconomic status, caregivers’ education, children’s gender, and service availability?
Detailed Findings
These findings build upon the interim evaluation report results published in 2018.
Nutrition Project Objective
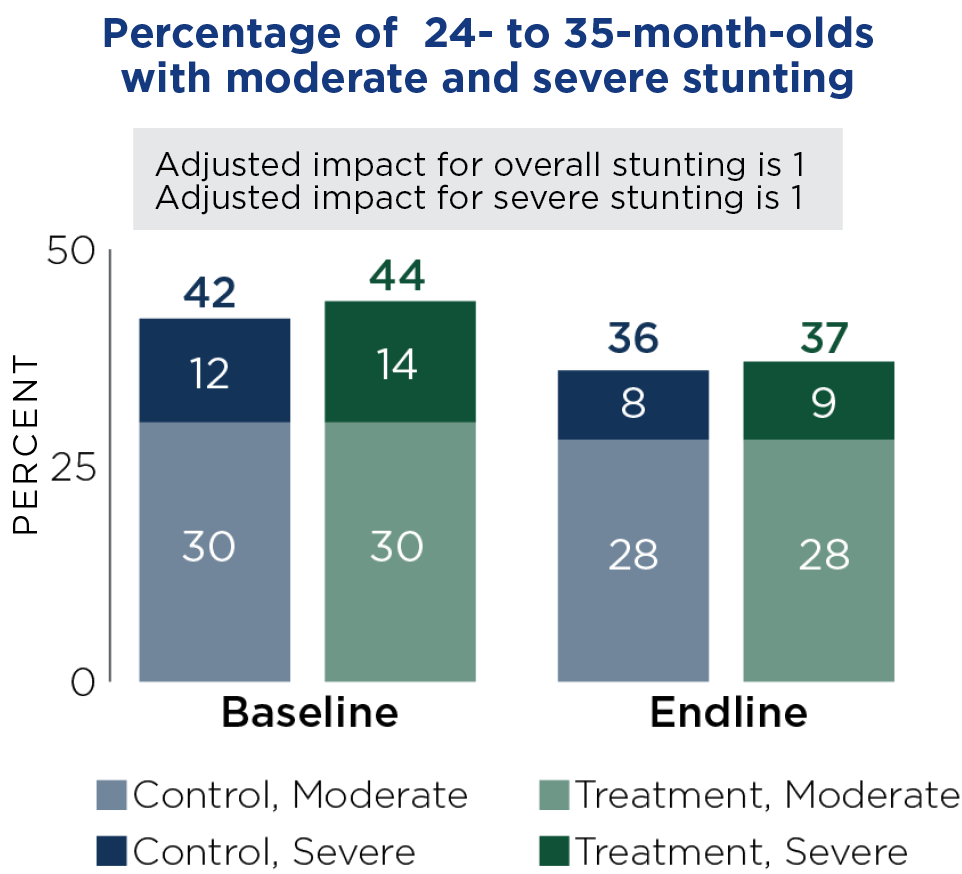
The project’s key long-term outcome was to improve health and nutritional status among pregnant women and children, as measured by rates of child stunting, wasting, underweight, and low birthweight. However, the project had no impact on these outcomes, even for the cohort with the most project exposure, although stunting declined in both treatment and control areas (see figure). These findings are consistent with the limited impacts on the sanitation- and nutrition-related outcomes described below, which were expected to drive changes in stunting. The project also showed no impact on stunting for subgroups and no evidence of a systematic pattern of impacts on any other outcome by subgroup.
Given the lack of impact of project interventions on key intermediate outcomes, it was not possible to determine which elements were the drivers of impact to answer the second evaluation question.
Sanitation-Related Intermediate Outcomes
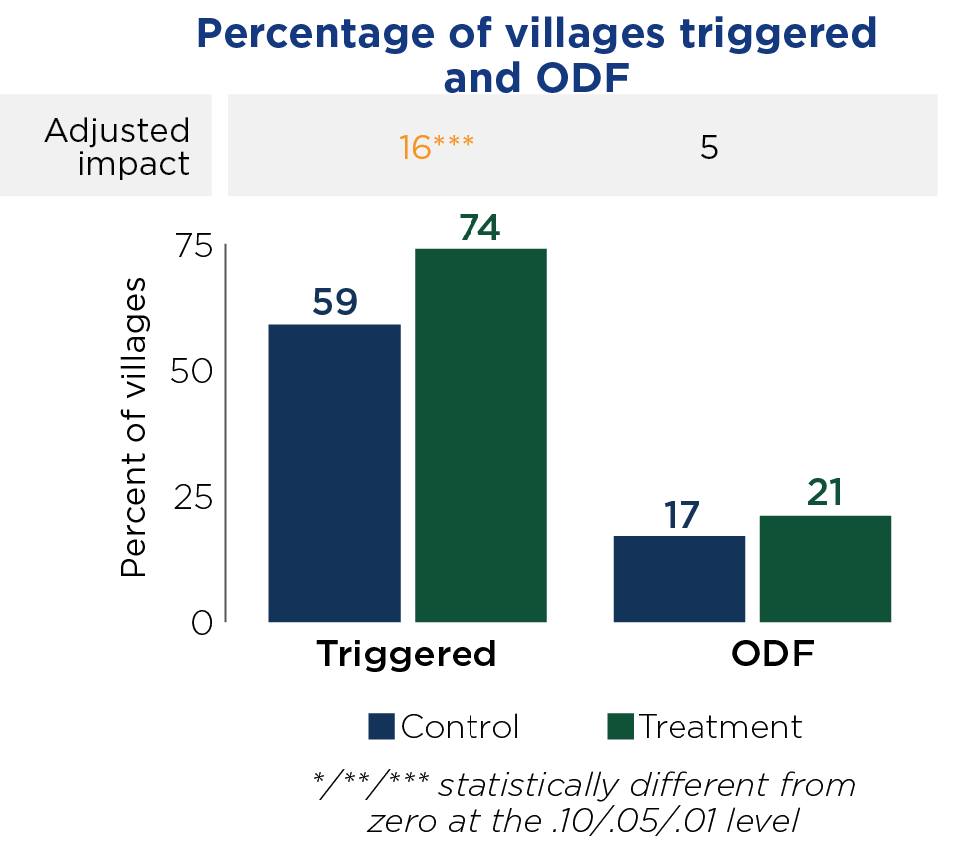
Because of the association between undernutrition and intestinal infections, the Nutrition Project sought to improve sanitation behaviors by mobilizing communities to address open defecation (through inter- active community gatherings known as “triggering”) and become open-defecation free (ODF).
The project had a positive impact on the percentage of villages that were triggered. On average, sanitarians in treatment areas reported that about 74 percent of villages that they oversee had been triggered, a statistically significant 16 percentage points higher than in control areas (see figure). However, the proportion of villages that had been verified as ODF was low in treatment areas—about 2 in 10—and similar to control areas. Consistent with the lack of impact on ODF, the project had no impact on the types of sanitation facilities reported by households, their sanitation-related behaviors, or the incidence of child diarrhea or worm infections.
Nutrition-Related Intermediate Outcomes
The Nutrition Project sought to achieve its key long- term outcome by improving a broad range of health outcomes during pregnancy and in the first two years of life. However, the project had limited effects on maternal and child service utilization and access, as intended by the community-driven development component, Generasi. It had no impact on receipt of one-on-one counselling during prenatal or postnatal checkups, or on the percentage of deliveries assisted with a skilled provider. The project affected the likelihood of women attending nutritional counseling sessions (by eight percentage points for pregnant women and seven percentage points for caregivers of young children), but overall attendance at nutritional counseling sessions remained low.
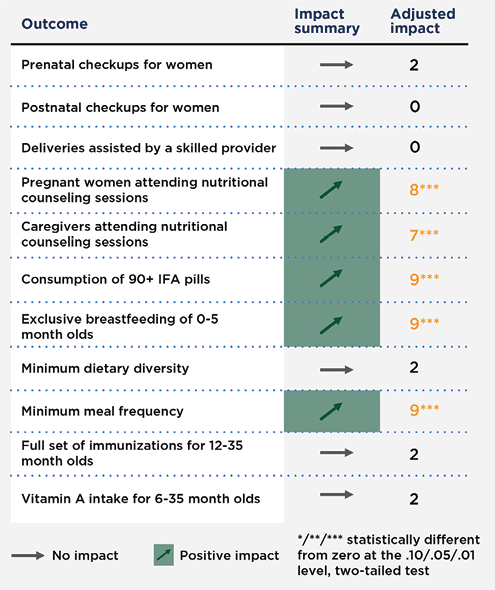
The project had statistically significant impacts on some nutrition-related outcomes, but these were modest in size. Specifically, it improved the likelihood of pregnant women consuming the recommended 90 IFA tablets during pregnancy, by nine percentage points, likely through the provision of IFA to district health offices. Similarly, it improved the likelihood of exclusive breastfeeding, also by nine percentage points. Although it had had no impact on minimum dietary diversity, it improved the treatment group’s minimum meal frequency by nine percentage points compared to the control group. There was no impact on immunizations or receipt of Vitamin A.
The evaluation also examined project impacts on all key outcomes by subgroups, including those defined by socioeconomic status, caregivers’ education, children’s gender, and service availability, as well as by province and cohort. Although there were substantive differences in impacts among certain subgroups for certain outcomes, the analysis did not identify any patterns that suggested that impacts were systematically different for particular subgroups.
Economic Rate of Return
MCC considers a 10% economic rate of return (ERR) the threshold to proceed with an investment
- 13%
Original ERR (2011) - 16.5%
Updated ERR (2013) - 0%
Evaluation-Based ERR (2019)
The evaluation-based ERR is substantially lower than the original ERRs for three main reasons. First, key activities driving the original ERR estimate were not implemented or faced major challenges. Second, fewer cohorts of children were exposed to the project activities than anticipated because of implementation delays. Third, the largest benefit streams in the original ERR estimate were driven by reductions in child diarrhea and stunting, which largely did not materialize.
MCC Learning
Ensure that MCC and the partner government are aligned in terms of the objectives of the project and obtain commitments from the involved government implementing entities before embarking on a project.
Develop and document the project’s detailed design and implementation arrangements prior to entering the compact implementation period.
Evaluation Methods
Mathematica conducted an impact evaluation of the Nutrition Project using a randomized controlled trial in the three newly added provinces of the 11 in which the project was implemented. The final evaluation relies on quantitative endline data collected by SurveyMETER approximately one year after the end of the project. It reflects an exposure to treatment of up to three years that varied by community and intervention. Impacts are regression-adjusted differences between treatment and control.
2020-002-2352


